- Acute pain most commonly occurs after surgery, as a result of injury or due to an acute medical illness.
- Managing your pain at home is an important part of your recovery.
- The aim of treatment is to reduce your pain to a level that allows you to return to your regular day-to-day activities.


Managing your pain medicines at home
A guide for short-term treatment of acute pain.
This information is intended for adult patients, and it explains how to use your prescribed pain medication, both safely and effectively at home.This information is intended for adult patients, and it explains how to use your prescribed pain medication, both safely and effectively at home.
Medicines for reducing pain
- Many medicines work in different ways for reducing pain.
- Using a combination of simple pain therapies like paracetamol and anti-inflammatory medicines, may allow for lower doses of, or no need for, strong pain medicine. This reduces the risk of unwanted side effects of strong pain medicines.
- There are many ‘brand’ names, forms and strengths for the same type of pain medicine and this can cause confusion. Check with your pharmacist if unsure.
Before you take pain medicine, tell your doctor or pharmacist if you:
- Have any allergies to medicines, especially pain medicines.
- Have any other medical conditions.
- Are pregnant or breastfeeding.
- Take other regular medicine or herbal supplements.
How to use your prescribed medicine safely and effectively at home
Paracetamol
Paracetamol 500mg, Paracetamol slow-release 665mg.
Paracetamol is a safe and well-tolerated medicine. It helps ease mild to moderate pain.
There are many brands of paracetamol. It is also available combined with other pain relief medicines and in cough and cold products. Avoid using more than one product containing paracetamol at the same time. Too much paracetamol can cause liver damage. If you are unsure if a product contains paracetamol, check with your pharmacist.
The maximum daily dose of paracetamol is 4000 mg. In some patients a lower daily dose is recommended.
Anti-inflammatory medicines
Celecoxib, Diclofenac, Ibuprofen, Indomethacin, Meloxicam.
Anti-inflammatory medicines reduce inflammation (swelling) and provide relief from mild to moderate pain.
They are generally well tolerated. In some people, they can cause stomach pain, reflux, gas or diarrhoea. Taking your medicine with a meal may help this.
Strong pain medicines
Opioid medicines are a form of strong pain medicine. The management of severe pain may require opioid medicines in addition to paracetamol and/or anti-inflammatory medicines. Opioid medicines should be used for the shortest time possible as they can be habit-forming.
Note: Long-term use of strong pain medicines (opioids) increases the risk of harms such as dependence and overdose. If you continue to have pain, or find it hard to stop taking pain medicines, see your doctor for a review.
Fast acting opioids
Oxycodone IR, Tapentadol IR, Tramadol IR, Codeine, Morphine IR.
Fast acting opioids, also known as immediate-release (IR) opioids, are the preferred opioid formulation for acute pain.
They work quickly to help strong intolerable pain, when other medicines like paracetamol or anti-inflammatories are not effective by themselves.
Note: Long acting opioids are also known as slow-release (SR) opioids, (e.g. oxycodone/naloxone SR, oxycodone SR, tapentadol SR, tramadol SR, morphine SR), and are reserved for the management of prolonged pain in some conditions.
Long acting opioids must be SWALLOWED WHOLE. Chewing, crushing, breaking or dissolving can be dangerous and cause serious problems, such as overdose.
Common questionsCommon questions
Common side effects of opioids are drowsiness, constipation, dizziness, nausea and vomiting.
- Because opioids can make you drowsy (sleepy), do not drive, drink alcohol or take sleeping tablets. Let your doctor know if you are taking other medicines that also make you feel sleepy.
- Do not take more tablets than you have been prescribed.
Stop taking your opioid medicine if you are very drowsy or having trouble staying awake. Go to the emergency department of your nearest hospital or call triple zero (000).
Constipation is common when using opioids and this may cause great discomfort.
Reduce the risk of constipation by:
- Drinking plenty of water.
- Maintaining a diet high in fibre.
- Increasing your physical activity (if appropriate).
- Taking a laxative (such as Macrogol or Docusate with Senna) regularly for the duration of your opioid therapy.
- Store medicines in a safe place, out of eyesight and out of reach of children.
- Don’t keep your strong pain medicines ‘just in case.’ Return unused opioids to your local pharmacy for safe disposal.
Pain normally gets a little better each day as you recover and your body heals.
You can reduce the amount of pain medicine you take in steps:
- Stop taking your strong pain medicines first – Reduce the dose of your opioid medicine a little each day according to your pain needs, and then stop.
- Take your anti-inflammatories for the duration prescribed and then stop.
- Lastly stop your paracetamol.
Summary of helpful tipsSummary of helpful tips
- Only take your opioid medicine for the reason it was prescribed by your doctor and do not take more than the prescribed dose.
- Keep track of when you take your pain medicine, a diary or app may be useful.
- Because opioids can make you sleepy, avoid alcohol and do not drive or operate machinery.
- Let your doctor know if you are taking other medicines that also make you feel sleepy.
- Never share your medicines.
- It is important you store medications safely, particularly out of reach of children.
- Pain medicines should not be used once you have recovered. If you feel you still need pain medicines beyond this time, consult your doctor.
- Return unused medicine to your local pharmacy for disposal.
For more informationFor more information
- Speak to your GP, pharmacist or the hospital where you were treated.
- A consumer medicine information (CMI) leaflet gives comprehensive information about your medication. You can ask your pharmacist for a printed copy, or search for a CMI leaflet via this website – www.healthdirect.gov.au/medicines.
- Phone Healthdirect on 1800 022 222.
- In case of overdose or poisoning, contact the 24 hour Poison Information Centre on 13 11 26.
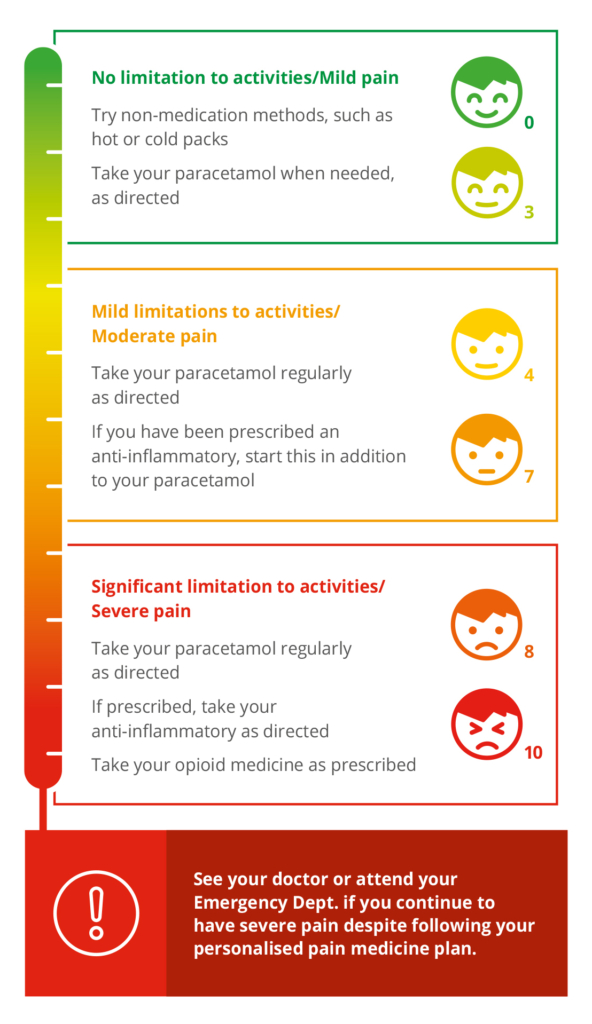
Pain Assessment and Management Plan
How is your pain affecting your day-to-day activities?
Give your pain a score (0 = no pain, 10 = the worst pain imaginable).
Disclaimer: This information is intended as a guideline only. It reflects the consensus of the authors at the time of publication. The sources used are believed to be reliable and in no way replace consultation with a health care professional.
Download your free brochure
Be informed, feel empowered. Our free brochure will help you make decisions about your, or your loved ones, care.

